The following is a guest article by Gayatri Thakkar, Founder and CEO at Inferenz
A Quiet Miss that Turned Serious
Mrs. Harris waited by the window for her morning wound check. The caregiver who knew her routine had a long commute and a flat tire.
The home care office tried to find cover with calls and texts.
Noon came. Then a fever.
By evening, her daughter drove her to urgent care.
No one meant for this to happen. The system in place missed the fact that the caregiver would have to travel quite a distance, and in any unforeseen situation, it would be hard to fill the care gap in time.
The Bigger Problem in Home Care Today
Stories like Mrs. Harris’s are common in U.S. home care. Agencies want to provide safe, reliable visits, but the systems they rely on are not built for today’s scale and speed. Healthcare establishments face rising demand, higher patient acuity, and a shrinking workforce. Yet, many still depend on outdated scheduling tools.
Most agencies use manual or rule-based systems. These tools work in calm conditions but collapse when anything changes, like a caregiver calling out or traffic delaying a nurse.
Key Challenges with Manual Scheduling:
- Fragmented Tools: Coordinators jump between phones, spreadsheets, EMRs, and HR systems to make a single change
- Slow Response: A last-minute call-out can take hours to cover, leaving patients waiting
- No Real-Time Data: Alerts in the EMR don’t always reach scheduling tools, so patients may be assigned caregivers without the right skills
- Geographic Blind Spots: Routes are often planned by static distance, ignoring live traffic or commute stress
- Burnout Risk: Uneven scheduling loads some caregivers with heavy cases and long drives, while others sit idle
For patients, this means missed or delayed care. For caregivers, it creates fatigue and frustration. For agencies, it drives turnover, penalties, and higher costs.
Why Scheduling Breaks for Both Sides
Patients Feel It
- Missed or late visits increase risk after surgery or a fall
- New orders sit unseen when tools do not talk to each other
- Trust slips when faces keep changing without notice
Caregivers Feel It
- Long back-to-back routes drain energy and raise injury risk
- Last-minute swaps create stress at home
- Unfair distribution of heavy cases pushes good people to leave
Schedulers Feel It
- Covering a call-out can mean five tools and two hours
- EMR alerts, skills, and travel all live in different systems
- Weekend scramble becomes the norm
What “Patient-Caregiver Matching” Actually Means
It is a simple idea. The patient caregiver matching solution fetches the latest data to assign the right caregiver to the right patient visit at the right time. Skills matter. Proximity matters. Language, preferences, and history matter. Do it fast and keep doing it as conditions change during the day.
Where AI-Based Smart Scheduling Helps
An AI scheduling layer sits on top of your existing EMR and agency software. It watches shifts, reads signals, and proposes or makes matches on its own when rules allow. Think of it as a digital coordinator that never gets tired.
Core Capabilities
- Reads live data from EMR, HR, maps, and messaging
- Scores fit for each open visit based on skills, history, and commute
- Sends offers to the best-fit caregivers in the right order
- If someone calls out, fills the gap in minutes and not hours
- Logs a clear reason for each match for audit and trust
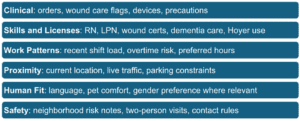
The Data Signals that Power Better Matches
Why Proximity-First Routing Lifts Retention
Shorter drives matter more than we admit. When the system favors close-by visits and logical chains, caregivers spend more time with people and less time on the road.
- Fewer long commutes mean lower stress
- More predictable days reduce no-shows
- A fairer spread of heavy and light cases builds trust
- New staff get steady hours near home, so they stay
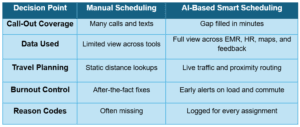
Manual vs AI-Based Scheduling at a Glance
When you compare how agencies handle scheduling today with what AI-based tools can do, the differences are clear. Manual methods depend on constant calls, scattered notes, and delayed updates, which leave both patients and caregivers exposed to risk.
An AI-driven approach, on the other hand, connects data streams in real time, reacts instantly to disruptions, and makes decisions with full context.
The table below highlights where the two models diverge most.
A Day in the Life with AI-Powered Smart Scheduling in Action
Imagine Sarah, a caregiver who has been with her agency for six years. Her mornings usually start with stress: long drives, uncertain assignments, and last-minute calls from the office.
But with smart scheduling in place, the picture looks different.
At 7:30 a.m., the system notices a new wound-care order for Mrs. Harris. Instead of leaving the office to scramble, it immediately ranks caregivers who have the right certification and live close enough to reach on time. Sarah’s name rises to the top.
By 8:10 a.m., the aide originally assigned calls in with a flat tire. Before anyone at the office can even pick up the phone, the system checks proximity, confirms Sarah’s wound-care skill, and sends her the offer. Two minutes later, she accepts. Mrs. Harris and her daughter receive a simple message: “Sarah is on her way, ETA 20 minutes.” What could have been another missed visit turns into a smooth hand-off.
Later that morning, the dashboard shows that two caregivers are running heavy back-to-back cases. The AI engine quietly adjusts the afternoon roster, routing easier visits to them and shifting the more complex cases to those with lighter loads. By 4:45 p.m., when a patient needs help refilling medication in Spanish, the system recognizes Sarah’s bilingual skill and redirects her nearby, sparing another patient the confusion of a language barrier. Sarah ends the day tired, yes, but not overwhelmed—because her hours, commute, and caseload are balanced with foresight rather than luck.
Guardrails that Keep the System Fair
Behind these smooth shifts is a framework designed to protect both staff and patients.
- Weekly hours are capped, licenses and scope of practice are locked into the rules
- Each match carries a plain explanation like “Assigned to Sarah for wound-care skill and two-mile commute”
- The system audits its own assignments every month, scanning for imbalance across staff groups, and it never blocks a human override
These checks make the AI a partner, not a replacement, in the work of care.
How to Roll Out the AI Solution Without Chaos
- Prepare the Data: Connect EMR, HR, timekeeping, and route data through secure APIs, clean key fields (skills, licenses, preferred hours, home zone, language)
- Start Small: Pick one branch or program for 8 to 12 weeks, let the system recommend while humans approve, move to auto-cover for call-outs once the team is comfortable
- Build Trust: Explain reason codes to staff, share early wins with real examples, invite feedback from caregivers and schedulers every Friday
- Expand With Care: Add more programs, turn on proximity-first chains, use insights to plan hiring for skills and locations that show recurring gaps
Features Checklist for the “Caregiver Connect” Solution
- Best-fit ranking for every open visit
- Proximity-first routing that reduces miles
- Skill and license matching tied to clinical rules
- Real-time call-out coverage with clear messages to all parties
- Fair-load signals that cool burnout before it spikes
- Reason codes and audit trail for each assignment
- Simple controls for human approval and exceptions
- Privacy and security aligned to HIPAA and your policies
What Patients and Caregivers Get
For patients, the difference is often felt in small but meaningful ways. Visits are less likely to be missed, and if a caregiver must cancel, another is assigned quickly without long gaps in care. The faces they see at the door are more familiar because the system favours continuity, sending caregivers who already know their case history, preferences, and routines. When changes do happen, patients and families receive timely updates, which removes the anxiety of waiting and wondering. This sense of reliability builds trust and keeps care on track.
For caregivers, the change is just as significant. Their workdays are shaped around logical routes that cut down on wasted travel, so the schedule makes sense both on paper and on the road. Instead of being overloaded with difficult cases while others sit idle, they receive a fairer balance of hours and patient types. The constant last-minute calls and schedule scrambles fade into the background, freeing up more energy for what matters most: the time spent with patients. This balance reduces stress, improves job satisfaction, and makes it easier for caregivers to stay in the profession longer.
Conclusion
Patient-caregiver matching brings order to one of the toughest parts of home care: scheduling. With AI guiding assignments, visits happen on time, caregivers feel supported, and leaders gain visibility into both cost and quality.
It creates a system where patients can count on continuity and caregivers can build sustainable routines. The outcome is a calmer office, stronger retention, and safer care delivered where it matters most, right where it is needed.
 About Gayatri Thakkar
About Gayatri Thakkar
Gayatri Thakkar is the Founder and CEO at Inferenz, a data and AI solution-led services company that primarily offers agentic AI solutions for multiple industries, especially healthcare. Owing to her two decades-worth of experience solving business problems with data and AI, she recently won the Silver award in the AI champions category at ISG Women in Digital Awards 2025 (APAC and India).


