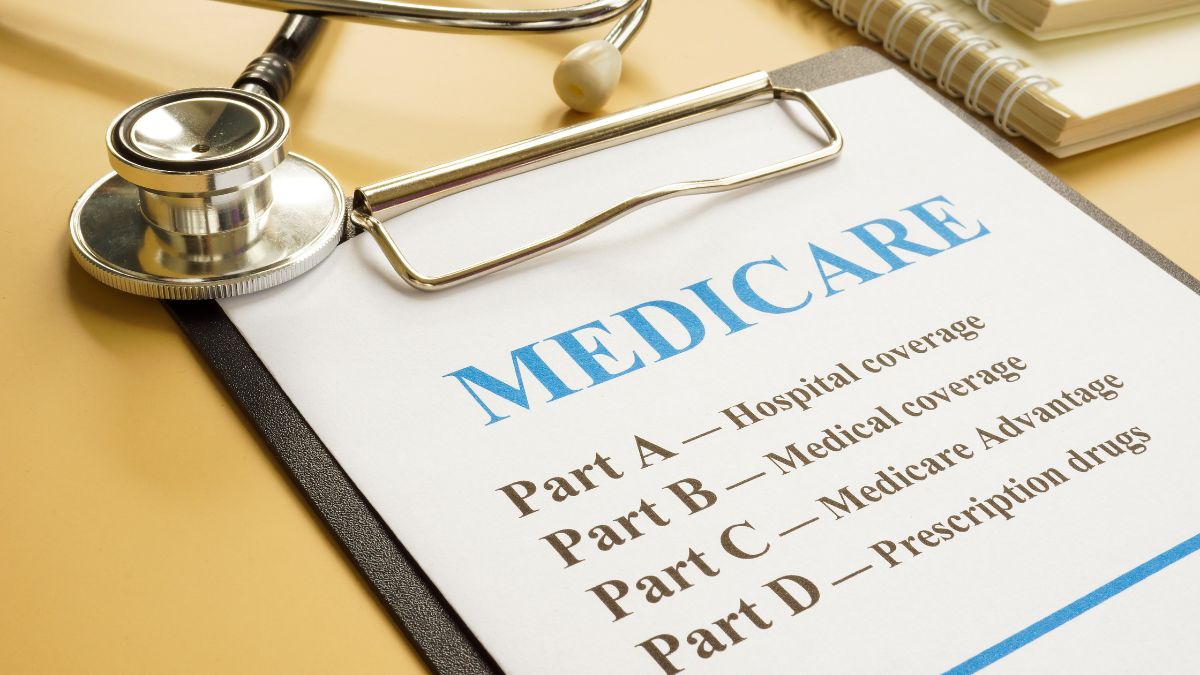
The Centers for Medicare and Medicaid Services (CMS) recently announced the launch of a program that will require individuals on Medicare to obtain prior approval from the federal health insurance program before undergoing certain procedures. It’s expected to start in 2026 in six states and will help “patients and providers avoid unnecessary or inappropriate care and safeguarding federal taxpayer dollars,” according to a CMS statement. Below, we break down exactly what this means for people on Medicare.
What to know about the Medicare prior authorization update
In June of this year, CMS announced that it would be launching the Wasteful and Inappropriate Service Reduction (WISeR) Model, which will require “prior authorization” for people on Medicare hoping to undergo certain procedures.
It will begin on January 1, 2026, and last for six years, with an expected launch in Arizona, New Jersey, Oklahoma, Ohio, Texas and Washington. They will then select certain companies in these states to test out the program.
“CMS is committed to crushing fraud, waste and abuse, and the WISeR Model will help root out waste in Original Medicare,” CMS Administrator Mehmet Oz, MD, said in a statement on the agency’s website. “Combining the speed of technology and the experienced clinicians, this new model helps bring Medicare into the 21st century by testing a streamlined prior authorization process, while protecting Medicare beneficiaries from being given unnecessary and often costly procedures.”
CMS also states that the services affected “include, but are not limited to, skin and tissue substitutes, electrical nerve stimulator implants and knee arthroscopy for knee osteoarthritis. The model excludes inpatient-only services, emergency services and services that would pose a substantial risk to patients if significantly delayed.”

Following the initial announcement, several members of Congress wrote a letter to Dr. Oz, arguing that “WISeR will likely limit beneficiaries’ access to care, increase burden on our already overburdened health care workforce and create perverse incentives to put profit over patients.”
“Traditional Medicare has rarely required prior authorization. This is vastly different in Medicare Advantage, in which beneficiaries are regularly subjected to prior authorization, as documented by the Department of Health and Human Services (HHS) Office of Inspector General (OIG) and CMS.2,” the letter states. “While prior authorization is often described as a cost-containment strategy, in practice it increases provider burden, takes time away from patients, limits patients’ access to life-saving care and creates unnecessary administrative burden. Many patients choose Traditional Medicare because they know their care will be determined by their doctors and not by insurance companies.”
They also requested clarification on how CMS selected the six states, how patients and providers will be informed of the change and other details. As of the time of publication, the agency has not commented on these inquiries.
Experts share how the prior authorization process could impact you
If you live in one of the six states selected for the authorization process and are looking to undergo one of the medical producers, Jeremy Gurewitz, cofounder and patient advocate at Solace Health, recommends ensuring “your doctor provides detailed medical records, imaging and clinical notes up front — approvals typically rest on proper documentation.”
“If Medicare denies your application, it’s not the end of the story: You have a right to appeal, and many denials are overturned when the applicant provides additional evidence,” he continues.

CMS has stated: “The WISeR Model will not change Medicare coverage or payment criteria. Health care coverage for Original Medicare beneficiaries remains the same, and beneficiaries retain the freedom to seek care from their provider or supplier of choice.”
The agency notes, “Model participants will receive payments based on their ability to reduce unnecessary or non-covered services (inappropriate utilization) and lower spending in Original Medicare. Participants’ payments will be adjusted based on their performance against established quality and process measures that measure the model participants’ ability to support faster decision-making for providers and suppliers and improve provider, supplier and beneficiary experience with the prior authorization process.”
Currently, it’s unclear how many people will be affected by this change. It’s also unclear if, once the trial phase ends in 2031, it will extend to other states.